
Glioblastoma, one of the most difficult cancers to treat
Glioblastoma is the most aggressive form of brain cancer with more than 250 000 new cases per year worldwide, and is considered incurable. With the best current treatment strategies, the average life expectancy after a diagnosis is 12-18 months – only 25% of patients survive more than a year, and only 5% of patients survive more than five years. The low survival rate is partly due to the blood-brain barrier, which protects the brain from unwanted substances. Due to the efficacy of this barrier, many drugs cannot be used to treat cancer in the brain at all, and others, such as temozolomide, needs to be administered in extra high doses, which leads to increased toxicity and side effects from the treatment. In GBM patients, the BBB is often disrupted (known as the blood–brain tumor barrier, BBTB) being much more permeable, so it is not usually considered as a main factor for therapy failure.
One of the major reasons for therapy failure is the resistance mechanisms mediated by the DNA repair protein (MGMT). In the project we propose the combination of two drugs, TMZ and an inhibitor of MGMT protein. Brain targeting NPs are advantageous here to avoid the accumulation of both drugs in healthy tissues that would occur after systemic administration of free drugs to avoid exacerbating the toxicity of the drug in the healthy tissues, and also to avoid variations in their relative concentration over time due to differences in their distribution and life-time in the body. In addition, current treatment strategies rely on daily administration of drugs over 6 weeks, which requires patients to either stay at or within close proximity to a hospital, further exacerbating the recovery process. Thus, there is a need for new and better therapies to combat this deadly form of brain cancer.
The solution
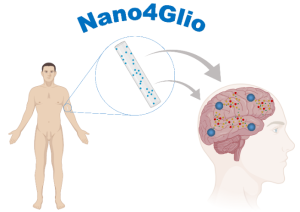
Nano4Glio: Engineered nano-based device for glioblastoma multiforme therapy is a 3-year M-ERA.NET financed researcher project coordinated by the University of Porto, with consortium partners i3S – Institute for Research and Innovation in Health, SINTEF and the University of Copenhagen. Nano4Glio will develop a new strategy composed of a biodegradable hydrogel incorporating drug-loaded nanoparticles (NPs) for GBM continuous treatment (see Figure). The drug-nanovehicle is expected to have a lifetime of 6 weeks, thus only requiring a single administration, eliminating the need for an extended hospital stay or daily commute to a treatment facility for the patient. Encapsulating the chemotherapeutic drug in nanoparticles which can cross the blood-brain barrier and reach the disease site efficiently allows for a continuous and enhanced therapy, while overcoming resistance. Thus, Nano4Glio will deliver a pioneering approach that will be able to overcome the limitations of current therapies.
The Team
The project team at SINTEF, led by Dr. Andreas Åslund, will contribute with their experience in development of implantable hydrogels suitable for incorporation and controlled release of nanoparticles. In addition to the SINTEF research team’s long experience with hydrogels and nanoparticles, Nano4Glio also ties in with an earlier SINTEF-financed strategic project on design of long-lasting implantable hydrogels led by Dr. Åslund (Long-lasting injectables for slow drug release). Nano4Glio is part of SINTEF’s strategic nanomedicine initiative which encompasses a wide range from the development of new particle systems to the encapsulation of drugs and the characterization of these nanomedicines physically, chemically, in cells (in vitro) and in animals (in vivo). Using nano-based vehicles to combat cancer is one of SINTEF’s prioritized areas within nanomedicine.
Sources:

















Comments
No comments yet. Be the first to comment!